 In the UK 350,000 people die from Cancer each year. One in two of us will be diagnosed with cancer at some point in our lives, according to a press release by Cancer Research in 2015. The statistic was previously one in three.
In the UK 350,000 people die from Cancer each year. One in two of us will be diagnosed with cancer at some point in our lives, according to a press release by Cancer Research in 2015. The statistic was previously one in three.
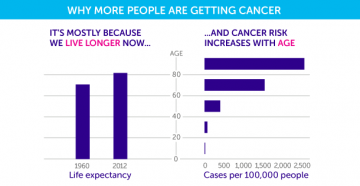
Cancer Research also suggest that people living longer is the main reason why the number has risen: “By far the biggest risk factor for most cancers is simply getting older. More than three-quarters of all people diagnosed with cancer in the UK are over the age of 60.
“And this is because cancer is a disease of our genes – the bits of DNA code that hold the instructions for all of the microscopic machinery inside our cells. Over time, mistakes accumulate in this code – scientists can now see them stamped in cancer’s DNA. And it’s these mistakes that can kick start a cell’s journey towards becoming cancerous.
“The longer we live, the more time we have for errors to build up. And so, as time passes, our risk of developing cancer goes up, as we accumulate more of these faults in our genes.”
Unless you have specific symptoms worrying you, or you’re part of a high-risk demographic then regular cancer screenings aren’t available through the NHS.
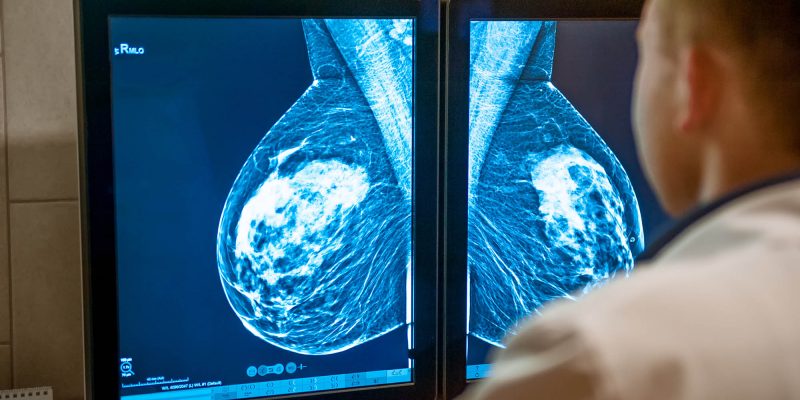
High-risk cancer groups include women aged 50-70 who are entitled to breast cancer screenings or ‘mammograms’ every three years.
Heidi Prentice is one of the women eligible to a mammogram screening: “I missed my first over 50’s mammogram because I moved town. I got the appointment through after about three years and I wasn’t sure about going at first as I was busy at work.
“I eventually went on the 29th of November in 2015, and thought I’d be sorted for the next three years. On the 7th December I received a letter saying that I’d been called back. I was sure I was in the 85% that would just be a cyst as the leaflet said.
“When I went for my appointment it was a whirlwind of ultrasounds and biopsies and I was completely shocked. I got called back and [I was] given the diagnosis that I had early, non-aggressive cancer in my left breast and it was treatable.”
After an operation, radiotherapy and a prescription of tablets to take for the next five years, Heidi considers herself to be lucky: “I have a massive dent in my left breast but I’m one of the lucky ones in two ways. I never knew I had a lump, it was found routinely. [Secondly] the lovely man I’m now married too didn’t walk away, as we met [eight months after I was diagnosed] and doesn’t mind I’m disfigured. I’m so lucky in so many ways.”
In the UK, standard screening is routinely available for few different cancers and high-risk groups of people. As well as breast cancer mammogram screening, regular smear tests are recommended and available for women aged 25, and bowel cancer screening for men and women aged between 60-74.
Prostate cancer screenings are recommended for men aged over 50 and are available on request to your GP. Other cancer screening is only carried out after sharing symptoms or concern with a medical professional like your doctor.
Apart from certain cases where screening has clearly worked for the individual, there is definitely concerns throughout the medical world on how effective they actually are overall. I spoke to Philip Rosell who is actively a surgeon and medical professional: “You run into the screening league time bias [which] is one of the technical terms for it. [That means] if you detect [cancer] earlier then you can treat it sooner. But it may not develop into full cancer, it may not spread, and the reason people are living longer is because you’re detecting it earlier.
“If you’ve got an average 2-3 years early detection, then [you have] 2-3 years increase in survival automatically, so there’s an element of a statistical trickery going on. The real question ‘does screening work?’ hasn’t been answered and politically it won’t be. [That’s] because politically we have breast cancer screening. The government is doing something about it. Any government that stopped it would be there be an outcry and accusations that you’re consigning women to death, whether it’s true or not. So, it’s a very emotive subject. But population screening is not necessarily the be all and end all.”
In the UK 350,000 people die of cancer annually. A low detection rate looms over the UK, compared to elsewhere in Europe, determined by research carried out by the Association of the British Pharmaceutical Industry (ABPI) in 2017, as well as various other studies.
I asked Philip about the poor UK cancer detection in comparison and if there are any misconceptions when it comes to the figures: “I worked in France and they are definitely more aggressive and more invasive with some things. Not necessarily because they’re trying to be fraudulent, it’s just their system. On the one hand they have a more privately led health service which is more customer demand led, and if you want a scan you can have a scan. In this country its more restricted.
“In most of Europe doctors are on fee for service, and if you’re being paid to do biopsies you will do more biopsies. If you’re being paid to do operations and you get paid more if it’s a cancer operation, you’ll do a lot more cancer operations, and that’s just the nature of the way the incentives work.
“Some of that is personality led, so as a country we tend to stiff upper lip, put up with stuff and don’t bother people, and certainly, the older generation are very much like that. I’ve seen women in their 80’s coming in with horrific advanced breast cancer which has completely destroyed a breast. The breast comes in looking like a cauliflower with lumps and bumps growing out of it, but they didn’t want to bother people because they’re a bit embarrassed.”
Read more of The 'C Word'...
 Bump to Mind – Perinatal Mental Health
Bump to Mind – Perinatal Mental Health