The Fertility Network UK and IVF Fairness are joining forces to campaign for an end to Britain’s IVF postcode lottery.
Dr Emily Scott from IVF Fairness said: “It’s a health equality issue and I hope that working alongside the Fertility Network and other lobbying organisations we can make a real change”.
The IVF postcode lottery refers to the current state of affairs in which clinical commissioning groups (CCGs) have sovereignty over what fertility services they will offer, who they are offered to and how many rounds each person is allowed.
In England, not only does your postcode determine your access to IVF but there is also a strict access criteria that can be a minefield for many couples hoping to start a family.
Spokesperson for the Fertility Network, Natalie Aminoff said: “We need to look at CCG’s because they are the ones who make the decision about funding and it can really impact someone’s whole life and their mental health.”
The postcode lottery has created huge inequalities up and down the country. There are vast differences between the services available from one CCG to the next.
In June – amidst huge backlash after the temporary suspension of fertility treatments in 2017 – the Cambridgeshire and Peterborough CCG decided to withdraw all NHS-funded fertility services.
The National Institute for Health and Care Excellence (NICE) guidelines recommend couples have access to three rounds of IVF, however the latest figures show 80% of CCGs do not currently offer this.
Former Junior Minister in the Department of Health, MP Jackie Doyle Price has said that the current system and postcode lottery “blights patients lives and damages the reputation of the NHS”.
During her time in the department for health Ms Doyle Price had “tried to ensure all CCGs offered at least one cycle of IVF.”

Figures obtained by one campaign group, Fertility Fairness, show that there are in fact seven CCGs that offer no NHS-funded fertility services at all.
CCGs were established as part of the Health and Social Care Act in 2012. They are groups of general practices in each area that commission services for their patients.
Since their creation, CCGs have faced criticism over their spending. The latest figures from the National Audit Office on the Financial sustainability of the NHS show that 32 out of 209 CCGs are facing a cumulative deficit and as a result are having to cut services.
General Practitioner, Dr Ruth Coleman said: “Unless we are willing to dig deeper into our pockets as tax-payers, then we really must start asking some difficult questions about what the NHS is for.
If we can’t afford to do everything then unfortunately fertility treatment is too close to the line and is the first thing that goes.
However, Dr Scott has argued that the World Health Organisation defines infertility as a disease and therefore the NHS should “treat it like one”.
Personal experience
Inspired by her own experience Dr Scott decided to start the petition to end the unfair and unequal access to IVF.
Unable to naturally conceive Dr Scott and her husband were advised by their GP to try IVF, being told they had access to three rounds on the NHS.
However, after three unsuccessful cycles and nearly one year later, they received an invoice in the post from the IVF clinic demanding £1,995 to be paid as soon as possible.
Dr Scott explained: “Before we started the treatment and the whole way through, we made sure that we were covered by the NHS for the treatment.”
Later, Dr Scott discovered that the Oxfordshire CCG policy that is shared with the Thames Valley area in which she falls under, offers only one round of IVF per couple.
In their summary of rationale for departing from NICE guidelines, a 2013 document released by the Thames Valley CCG states that the recommended assisted reproduction services would be “unaffordable”.
Having IVF can be a very difficult treatment with a gruelling six stage process to harvest a woman’s eggs. During in vitro fertilisation (IVF), an egg is removed from a woman’s ovaries and fertilised with sperm in a laboratory. Once fertilised, the embryo is placed in the woman’s womb to develop.
There is less than a 30% chance that IVF treatment will be successful for women aged 35 and under with success rates decreasing significantly with age.
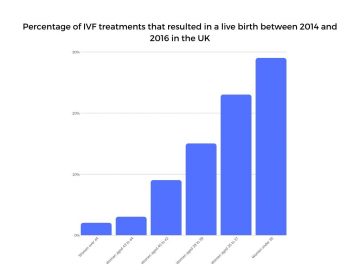
Scotland are currently leading the way in the UK for progressive fertility access for all, with three cycles of IVF per couple.
In England issues with the current access guidelines include secondary infertility (whereby you are unable to conceive a second child) not being acknowledged, as well as your age being a major factor in whether or not you are deemed eligible.
With the purse strings of the NHS tightening, Dr Coleman said: “You can only work with what you’ve got so you have to work with the system that your CCG has given you.
“I think if we wanted to be fair there is an argument that says no fertility treatment should be offered on the NHS.
We’re up against comparing it with ever more expensive drugs for cancer and that sort of thing and I think women are fortunate to get it for free at all.
In the UK more than 250,000 babies have been born through IVF since the birth of Louise Brown, the first IVF baby in 1978. Since then IVF success rates have improved but with CCGs continuing to deny fair and equal access to fertility treatment. This means that people across the country are being left to face the emotional, social and financial hurdles alone.
The future of the IVF postcode lottery
After the calling of the snap election on the 29th October, the IVF Fairness petition pushed to reach 100,000 signatures to ensure the issue of equal access to IVF would be discussed in the new parliament.
By the 6th November the petition reached 10,682 signatures and is currently waiting to be debated in parliament.
Reluctantly having to end their IVF journey and look at other paths to parenthood, Dr Scott said: “This isn’t going to help us now… But if we can change it and can help just one person, then at least all of this heart ache hasn’t just been for nothing.”

For help and support visit here.
More from this article:

 Protest music is for women too
Protest music is for women too